Hemogram Test: Complete Guide to the HGM Blood Test (Complete Hemogram/CBC)
Hemogram (also spelled haemogram) is a common blood test that provides a comprehensive overview of your blood’s cellular components. Often referred to as an HGM test or complete hemogram test, it measures the counts and characteristics of red blood cells, white blood cells, and platelets in your blood. In many cases, a hemogram test also includes the Erythrocyte Sedimentation Rate (ESR), giving additional insight into inflammation in the body.
This makes the hemogram a crucial screening tool for general health check-ups and for diagnosing a variety of conditions ranging from anemia and infections to clotting disorders and blood cancers.
In this in-depth guide, we will explain what a hemogram test means, how it compares to a standard Complete Blood Count (CBC), how to interpret a hemogram report, and why it’s significant. We’ll also cover the HMG test full form, the list of components in a complete hemogram test, the role of ESR, typical costs (hemogram test price) and factors affecting them, and answer frequently asked questions about haemogram testing.
What Is a Hemogram Test and Why Is It Important?
A hemogram test – sometimes simply called a hemogram blood test – is essentially a complete analysis of the cellular elements in your blood. The word “hemogram” literally means a record or picture of blood (“hemo-” for blood, “-gram” for record). In practical terms, this refers to a test that counts and examines different types of blood cells. By checking your red blood cell count, hemoglobin level, hematocrit, white blood cell count (and differential), platelet count, and other related parameters, a hemogram provides vital information about your overall health.
Significance: The hemogram is one of the most routinely ordered medical tests because of its broad diagnostic value. It can help detect conditions such as:
- ⚫ Anemia: Low hemoglobin or RBC counts can indicate anemia, leading to symptoms like fatigue and weakness.
- ⚫ Infections and Inflammation: High white blood cell counts or high ESR may suggest an ongoing infection or inflammatory process in the body.
- ⚫ Bleeding or Clotting Disorders: Abnormal platelet counts could point to bleeding tendencies or risk of excessive clotting.
- ⚫ Blood Cancers or Bone Marrow Disorders: Markedly abnormal counts (very high or very low) of certain blood cells can be an early clue for conditions like leukemia or lymphoma.
- ⚫ General Health Status: Even when no specific illness is suspected, a hemogram is useful for routine health check-ups to ensure all blood cell parameters are within normal ranges.
In essence, a haemogram test means doing a broad health screening of the blood – it helps doctors evaluate your immune system, oxygen-carrying capacity, and clotting ability all at once. Because blood circulates throughout every organ, abnormalities in blood counts often reflect underlying health issues. Early detection is a major advantage: for example, a simple hemogram might reveal mild anemia or an elevated white cell count before symptoms become severe, prompting further investigation or treatment. This is why doctors often include the hemogram in yearly physicals or pre-surgery evaluations – it’s a quick way to check for hidden problems.
Moreover, if you are undergoing treatment for a known condition (such as iron supplementation for anemia or chemotherapy for cancer), periodic hemogram tests help monitor your progress and response to therapy, indicating whether blood values are improving or if any side effects (like low counts due to medications) are occurring.
Hemogram vs. Complete Hemogram vs. CBC: Is There a Difference?
You might come across different terms like hemogram, complete hemogram, and CBC (Complete Blood Count). In most practical contexts, these refer to very similar (often identical) test panels, but there are subtle distinctions worth noting:
- ⚫ CBC (Complete Blood Count): A CBC is a widely used term, especially in international and scientific settings, for a blood test that counts the main types of cells in your blood. A standard CBC typically includes red blood cell count, white blood cell count (often with a breakdown of types, if a “CBC with differential” is ordered), hemoglobin, hematocrit, and platelet count. It focuses on the cellular elements without necessarily including the ESR. In other words, a CBC by itself usually does not include ESR.
- ⚫ Hemogram: In many parts of the world (including South Asia), the term hemogram or haemogram is used interchangeably with CBC. A hemogram generally includes everything in a CBC – counts of RBC, WBC (with differential), platelets, and calculated indices like MCV, MCH, MCHC, RDW (explained later). The key difference is that a hemogram often implies a more comprehensive panel that may include the ESR as well. Some labs and doctors use “hemogram” to mean CBC + ESR, considering it a more “complete” assessment. In fact, many diagnostic centers label their test package as “Complete Hemogram (CBC & ESR).”
- ⚫ Complete Hemogram: This term explicitly suggests that the test is a full hemogram with all components. In practice, “complete hemogram” usually means a CBC test plus the ESR measurement, and possibly a peripheral blood smear examination if needed. Essentially, it’s the most comprehensive form of a hemogram. However, often hemogram and complete hemogram are used synonymously, since a hemogram by definition is comprehensive. To avoid confusion, some labs stick to saying “CBC with ESR” for clarity.
In summary: A standalone CBC covers the blood cell counts and indices, while a complete hemogram typically covers everything the CBC does, plus the ESR. For example, if you order a hemogram test at many labs, you will get CBC results and an ESR reading in the report. If you order a CBC test, you might not get ESR unless specifically requested (or unless the lab uses the term interchangeably).
From a patient perspective, if your doctor writes a prescription for a hemogram or complete hemogram, you can expect to have one blood sample drawn and the lab will run both the CBC and ESR on it. On the other hand, if the doctor just says CBC, they likely only need the cell counts; an ESR could be added separately if needed. Always clarify with your healthcare provider or the lab if you’re unsure what will be included, but rest assured that haemogram test means an extensive blood count evaluation, and in many cases, it’s effectively the same as doing a CBC along with an ESR test.
Hemogram vs Hemoglobin Test: A quick note on terminology: do not confuse hemogram with hemoglobin test. Hemoglobin (Hgb) is just one component of the hemogram. A hemoglobin test measures the amount of the oxygen-carrying protein in your red blood cells and is often used specifically to screen for anemia. A hemogram, meanwhile, measures hemoglobin and much more. So, while hemoglobin level is part of a hemogram, the hemogram encompasses a complete blood count. If someone asks for an “Hb test” they mean just the hemoglobin; but if they say “HMG test” or “hemogram test,” they mean the entire panel of blood counts.
Hemogram vs. Complete Blood Picture (CBP): In some healthcare settings (especially in India), you might also hear the term Complete Blood Picture (CBP) or Complete Blood Profile. These are essentially synonyms for CBC/hemogram as well, emphasizing the idea of a full picture of blood cells. Different labs use different naming conventions, but the content of the test is largely the same.
To avoid any doubt: if you’re ever uncertain whether your “complete hemogram” includes the ESR or other components, just ask the lab or doctor. But by convention, hemogram = CBC + ESR in many labs, whereas CBC alone might omit the ESR. Both provide critical information, and together they offer a thorough assessment of your blood.
When and Why Is a Hemogram Test Recommended?
Because a hemogram test gives a broad snapshot of one’s health, it is recommended in a variety of situations. Here are some common scenarios and symptoms where a doctor may advise a hemogram:
- ⚫ Routine Health Check-ups: Many physicians include a complete hemogram as part of annual or periodic health check-ups. Even if you feel healthy, this test can detect issues like mild anemia or subclinical infection early. It’s a good baseline test for overall wellness.
- ⚫ Unexplained Fatigue or Weakness: If you’re experiencing persistent tiredness, weakness, or dizziness, a hemogram can check for anemia (low red blood cells/hemoglobin) or other issues that might cause such symptoms.
- ⚫ Fever or Signs of Infection: When you have a fever, especially if it’s high or prolonged, doctors often order a hemogram/CBC to see if your white blood cell (WBC) count is elevated (which can indicate an infection) and to check which type of WBC is high (neutrophils for bacterial infections, lymphocytes for viral, etc.). It can also identify signs of dengue or other illnesses that affect blood counts (like low platelets in dengue fever).
- ⚫ Bruising or Bleeding: If you have unexplained bruises, frequent nosebleeds, gum bleeding, or any signs of bleeding tendency, the hemogram will include a platelet count to see if it’s low (platelets help blood clot). A low platelet count could explain easy bruising or bleeding.
- ⚫ Inflammation, Joint Pain, or Body Aches: Symptoms like joint pains or generalized aches might prompt a test for inflammation markers. Along with other tests, a doctor might order a hemogram with ESR. A high ESR can signal significant inflammation in the body (seen in conditions like rheumatoid arthritis, autoimmune diseases, or severe infections).
- ⚫ Known Conditions Monitoring: If you have a known blood disorder or other medical condition, regular hemograms might be part of monitoring. For example, if you are on medication that can affect the bone marrow (such as certain anti-thyroid drugs, or chemotherapy for cancer), your doctor will check your CBC/hemogram frequently to ensure your WBCs, RBCs, and platelets are not dropping to dangerous levels. Diabetics or patients with kidney disease might also get periodic CBCs as part of their check-ups.
- ⚫ Pre-surgery or Hospital Admission: Before a surgery or any invasive procedure, doctors typically order a hemogram to make sure you’re not anemic (which could be a risk for surgery) and that your blood can clot normally (from platelet count) and to check for any unseen infection (via WBC count). It’s a standard part of pre-operative testing.
- ⚫ Sudden Weight Loss or Night Sweats: These can be red-flag symptoms for conditions like infections or even blood cancers. A hemogram may reveal abnormal cells or counts that require further investigation.
- ⚫ Assessment of Overall Health “Status”: Sometimes a hemogram is done simply because a patient hasn’t had any tests done in a long time. It acts as a broad sweep – if everything in the hemogram is normal, it’s reassuring that at least the blood cell component of health is in good shape.
Symptom Examples: To illustrate, consider someone who visits a doctor with complaints of persistent fever, fatigue, and body aches. The doctor orders a hemogram. The results show a high total WBC count and a high percentage of lymphocytes, as well as an ESR significantly above normal. This pattern might suggest a viral infection or even something like tuberculosis (which often raises ESR). Or if someone has fatigue and the hemogram comes back with low hemoglobin and low RBC count, it clearly points toward anemia as a cause. In each case, the hemogram guides the next steps – whether more tests are needed, or what treatment to start.
In children and pregnant women, hemograms are also common. During pregnancy, a CBC/hemogram is done in each trimester to check for anemia (which is common in pregnancy) and other issues. In children, if they have fever or appear pale or have unusual bruising, a CBC can be very telling.
Overall, the hemogram is such a fundamental test that it’s used both as a diagnostic tool when someone is ill and as a screening tool when someone is healthy. Its importance lies in its versatility – a single blood sample can reveal a lot about different systems of the body.
Also Read: Struggling with Hair loss? These Blood Tests Could Reveal the Cause
How Is the Hemogram Test Done? (Procedure and Preparation)
The procedure for a hemogram test is straightforward and minimally invasive. It involves a standard blood draw (venipuncture) which most of us have experienced. Here’s what to expect:
A lab technician performing a venipuncture, drawing blood into a purple-top collection tube (EDTA vial) typically used for hemogram/CBC tests.
- ① Sample Collection: A phlebotomist (trained technician) will tie a tourniquet (elastic band) around your upper arm to make the veins more prominent. After cleaning the skin with an antiseptic swab (usually alcohol) at the puncture site (often inside of the elbow), a sterile needle is inserted into a vein. You’ll feel a small pinprick. Blood is drawn into a tube – for a hemogram, the tube usually has an anticoagulant (EDTA) and is often colored purple or lavender on top, which prevents the blood from clotting so the cells can be counted accurately.
- ② During the Draw: The process only takes a minute or two. A small amount of blood (usually 2-5 mL, which is just a teaspoon or so) is enough for a complete hemogram. You might feel a slight sting or nothing much at all. It’s typically quick. If multiple tests are ordered, they may fill a couple of tubes. For just a hemogram, often a single tube suffices (since modern analyzers can run all the required measurements from one sample).
- ③ After the Draw: Once the tube is filled, the needle is withdrawn, and the technician will ask you to apply gentle pressure with cotton or gauze on the puncture site. They’ll usually put a small bandage or tape on it. It’s good to keep that on for 10-15 minutes and avoid heavy lifting with that arm for an hour or so to prevent bruising.
- ④ Lab Analysis: The collected blood is then sent to the laboratory. In the lab, an automated hematology analyzer machine processes the sample. These machines count the cells using methods like electrical impedance or laser flow cytometry, providing a printout of the counts and indices. The ESR, if included, may be measured either by a manual Westergren method (where the blood is placed in a vertical tube and the rate at which red cells fall is measured in mm/hour) or by an automated analyzer that can do ESR. Most large labs have automated systems, but the principle remains measuring how quickly RBCs settle in a tube.
- ⑤ Time for Results: Hemogram tests are typically quick to run. Many labs can return results the same day, often within a few hours if needed. If you’re inpatient in a hospital, CBC results can be ready in an hour or less. As an outpatient, you might get the report by end of day or the next day. Some diagnostic centers now even offer home collection services (a phlebotomist comes to your home to draw the blood) and then email the hemogram test report to you the next day, which is very convenient.
Preparation for the Test: One of the benefits of a hemogram is that no special preparation is usually required. You do not need to fast for a CBC/hemogram – unlike cholesterol or glucose tests that require fasting, a hemogram is unaffected by recent meals. You can eat and drink normally before the test. However, some doctors might club the hemogram with other tests that do require fasting (like blood sugar or lipid profile). In such cases, you might be asked to come fasting so that all tests can be done from one blood draw. But for the hemogram itself, fasting is not needed.
A few practical tips:
- ⚫ Hydration: It’s good to be reasonably well-hydrated before any blood test. Being hydrated can make your veins easier to find and may make the blood draw faster. Simply drinking water as you normally would is fine.
- ⚫ Medications: Generally, you continue your routine medications unless instructed otherwise. Certain medications can influence blood counts (for example, steroids can raise WBC, some drugs can lower WBC or platelets), but you should not stop any prescription medication without advice. Just ensure your doctor knows what you’re taking; they will interpret results with that in mind. If you are taking over-the-counter supplements (like iron, vitamins), it usually doesn’t interfere with the test, but again, let the doctor know if they have any questions.
- ⚫ Relax: Being calm can help, especially if you’re prone to anxiety around needles. The procedure is quick, and taking slow breaths or looking away if you dislike the sight of blood can help.
Risks and Aftercare: The hemogram test is very low-risk. Aside from the slight prick of the needle, you might have a tiny bruise or soreness at the puncture site for a day. Serious complications like infection or significant bleeding from the draw site are exceedingly rare when proper procedure is followed. If you have a bleeding disorder, you should inform the technician, but even then, the small gauge needles used usually don’t cause issues.
If you feel lightheaded after any blood draw (some people do if they’re anxious or have a vasovagal response), inform the staff and take a few minutes to rest. It’s wise to not stand up too quickly if you feel woozy. But for the vast majority, a hemogram blood test is a routine, quick procedure with no downtime – you can resume normal activities immediately afterward.
Components of a Complete Hemogram Test (List of Parameters)
A complete hemogram test report contains a list of various parameters that together paint a picture of your blood’s composition. Here is the complete hemogram test list of components and what each means:
- ⚫ Red Blood Cell (RBC) Count : This is the number of red blood cells in a given volume of blood (typically reported as million cells per microliter). RBCs are the cells that carry oxygen from your lungs to tissues via hemoglobin. The hemogram measures the RBC count to see if it’s within normal range. A low RBC count suggests anemia or blood loss, whereas a high RBC count could indicate polycythemia (which can occur due to bone marrow disorders or chronic low oxygen levels, as in heavy smokers or high-altitude dwellers).
- ⚫ Hemoglobin (Hb or HGB): Hemoglobin is the iron-containing protein in red blood cells that actually carries oxygen. This value, measured in grams per deciliter (g/dL), is crucial – it directly indicates the blood’s capacity to carry oxygen. It’s often the primary number doctors look at for anemia. Low hemoglobin = anemia; high hemoglobin can occur in dehydration or polycythemia. Hemoglobin typically correlates with RBC count but is a more direct measure of oxygen-carrying capacity.
- ⚫ Hematocrit (Hct or PCV): Hematocrit, also known as Packed Cell Volume (PCV), is the percentage of your blood volume that is made up of red blood cells. If you imagine spinning blood in a centrifuge, the red cells pack down at the bottom; hematocrit is the fraction of the tube that is red cells. It is given as a percentage. Low hematocrit indicates anemia (fewer cells in blood, more plasma proportionally), while high hematocrit indicates a high concentration of RBCs or reduced plasma (could be due to dehydration or conditions like polycythemia). Hematocrit typically is roughly three times the hemoglobin value (for example, Hb of 15 g/dL corresponds to Hct ~45% in a healthy person).
- ⚫ Red Blood Cell Indices: These are calculations that describe the size and hemoglobin content of the average red blood cell:
- ⦿ Mean Corpuscular Volume (MCV): the average size (volume) of a red blood cell, measured in femtoliters. This tells whether RBCs are normal-sized, too large (macrocytic), or too small (microcytic). For instance, iron deficiency anemia often causes low MCV (microcytic anemia), whereas vitamin B12 deficiency causes high MCV (macrocytic anemia).
- ⦿ Mean Corpuscular Hemoglobin (MCH): the average amount of hemoglobin in a single red blood cell (in picograms). It often parallels MCV – macrocytic cells have more hemoglobin, microcytic have less – but MCH is less commonly focused on than MCV and MCHC.
- ⦿ Mean Corpuscular Hemoglobin Concentration (MCHC): the average concentration of hemoglobin inside the red cells (g/dL). It indicates how “full” of hemoglobin the cells are. In some anemias, cells can be paler (low MCHC, called hypochromic, e.g., in iron deficiency) or normal (normochromic).
- ⦿ Red Cell Distribution Width (RDW): a measure of the variation in size of the RBCs. If RDW is high, it means there’s a wide range of RBC sizes (anisocytosis) – for example, some very small, some normal – which can happen in mixed deficiency anemia or recovering anemia. A normal RDW means most RBCs are about the same size.
- ⚫ These indices help doctors narrow down causes of anemia. For instance, a low MCV, low MCH anemia (microcytic, hypochromic) often points to iron deficiency or thalassemia, whereas a high MCV anemia might point to B12/folate deficiency or alcoholism, etc. They are part of the automated report and add depth to interpretation, though for a layperson, it’s enough to know they describe RBC characteristics.
- ⚫ Total Leukocyte Count (TLC) / White Blood Cell (WBC) Count: This measures the total number of white blood cells in a volume of blood (typically given as cells per microliter or thousands per microliter). WBCs are the immune cells that fight infection, and include several different types (neutrophils, lymphocytes, etc., described below). A normal WBC count in adults is roughly 4,000-10,000 per microliter. If the WBC count is high, it’s called leukocytosis – common causes include infections (especially bacterial), inflammation, trauma, or leukemia (a type of blood cancer). If the WBC count is low (leukopenia), it can be due to certain viral infections, bone marrow problems, or as a side effect of medications. The hemogram will give you the total WBC count and often flags it as high or low if outside the normal range.
- ⚫ WBC Differential Count: This breaks down the white blood cell count into the different types of leukocytes, typically given in percentages (%) and sometimes in absolute numbers (absolute count per microliter) for each type. The main types are:
- ⦿ Neutrophils: These are the most abundant type of WBC and the first responders to bacterial infections. Normal neutrophil percentage is roughly 40-70% of WBCs. A high neutrophil count (neutrophilia) often indicates bacterial infection or acute inflammation; a low count (neutropenia) can increase infection risk and may result from certain medications or bone marrow issues.
- ⦿ Lymphocytes: These cells are crucial for viral defense and include B-cells and T-cells. Normal range is about 20-40% of WBCs. High lymphocytes (lymphocytosis) might indicate viral infections like mononucleosis or chronic infections/tuberculous, and certain leukemias (like CLL). Low lymphocytes (lymphopenia) might occur due to immunosuppressive conditions or severe stress.
- ⦿ Monocytes: These are larger immune cells that become macrophages in tissues, cleaning up debris and fighting certain infections like tuberculosis. Normal range ~2-10%. Monocytosis (high monocytes) can be seen in chronic infections, inflammation, or recovery phase of acute infection.
- ⦿ Eosinophils: These are involved in allergic reactions and fighting parasites. Normal eosinophil count is small, ~1-6%. Eosinophilia (high eosinophils) commonly suggests allergies (like asthma, hay fever) or parasitic infections; it can also be elevated in certain skin diseases or drug reactions.
- ⦿ Basophils: The rarest WBC type (~0-1% normally). They play a role in allergic responses and release histamine. Basophilia (high basophils) is uncommon but can be seen in certain blood disorders or allergic inflammation.
- ⦿ The differential can be reported in two ways: relative (%) and absolute count. The absolute counts (which the analyzer often provides, e.g., Neutrophils 3000/µL, Lymphocytes 2000/µL, etc.) are more clinically useful, because the percentage can be misleading if total WBC is very high or low. Many lab reports will list both, or at least the percentage. For interpretation, doctors often look at the absolute values.
- For example, a hemogram might report: “WBC 12,000 (Neutrophils 80%, Lymphocytes 15%, Monocytes 3%, Eosinophils 2%, Basophils 0%)”. This tells the doctor that neutrophils are not only high in percent but also in absolute number (~9,600 in this case, which is above normal), likely pointing to an acute bacterial infection.
- ⚫ Platelet Count (Plt): Platelets (also called thrombocytes) are tiny cell fragments crucial for blood clotting. The normal platelet count is about 150,000 to 450,000 per microliter of blood. The hemogram measures how many platelets you have:
- ⦿ Thrombocytopenia: If platelets are low (below 150k), one may bruise easily, have nosebleeds or bleeding gums, or in very low cases (<20k>
- ⦿ Thrombocytosis: If platelets are high (above 450k), it could be reactive (due to inflammation, infection, or recent surgery) or due to a bone marrow disorder (like essential thrombocythemia). High platelets can sometimes increase the risk of clotting (though if extremely high, paradoxically can also cause bleeding issues due to platelet dysfunction).
- ⚫ Platelet counts can fluctuate and often labs will recheck an abnormal platelet count to confirm (since platelets can clump and cause false low readings occasionally). The hemogram often also reports platelet indices like Mean Platelet Volume (MPV), which indicates the average size of platelets. An elevated MPV means platelets are larger on average (often when the bone marrow is rapidly producing platelets, they come out bigger). Other platelet indices include PDW (platelet distribution width), but these are more of academic interest and not typically something patients need to focus on in the report.
- ⚫ ESR (Erythrocyte Sedimentation Rate): ESR is often reported separately in a hemogram test report (sometimes at the bottom or on a second page) because the method of measurement is different. ESR is measured in millimeters per hour (mm/hr) and indicates how quickly red blood cells settle in a vertical tube over one hour. We’ll discuss ESR in detail in the next section, but in brief: a normal ESR is usually quite low (e.g., 0-10 mm/hr for men, 0-20 mm/hr for women, with slightly higher values possible in the elderly). A high ESR means the red cells are settling faster, which usually happens when there are increased inflammatory proteins in the blood. It’s a nonspecific marker of inflammation or infection. In a “complete hemogram with ESR”, you will get this value alongside the CBC.
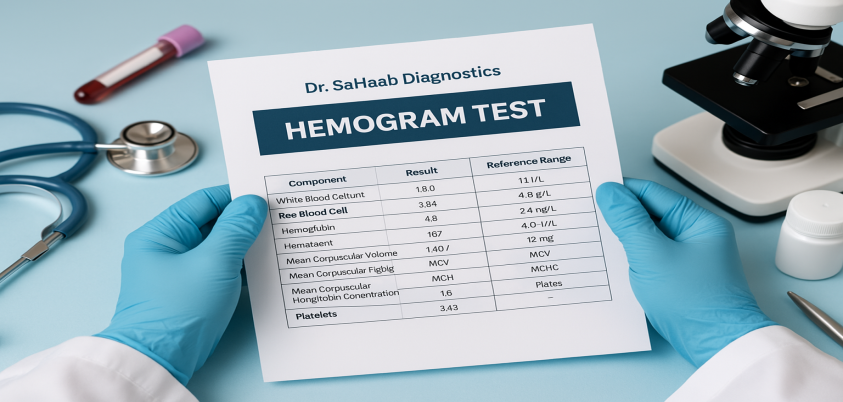
These components together form the complete hemogram test list. On your hemogram report, you’ll typically see each of these parameters with a result value and a reference range (normal range) next to it for comparison. For instance, it may show:
- Hemoglobin: 14.0 g/dL (Normal range: 13.0–17.0 g/dL for males)
- Total WBC: 7,500 per µL (Normal: 4,000–10,000)
- Neutrophils: 55% (Absolute 4,125 per µL)
- Lymphocytes: 35% (Absolute 2,625 per µL)
- Monocytes: 7% (Absolute ~525 per µL)
- Eosinophils: 3% (Absolute ~225 per µL)
- Basophils: 0% (Absolute 0)
- RBC count: 5.0 million/µL
- Hematocrit: 45%
- MCV: 90 fL
- MCH: 30 pg
- MCHC: 33 g/dL
- RDW: 13%
- Platelet count: 250,000/µL
- MPV: 8.5 fL
- ESR: 10 mm/hr
(This is an example of a healthy adult’s possible report values – within normal limits.)
Each lab’s report format might differ slightly. Some combine RBC, Hb, Hct in one section, WBC and differential in another, platelets separately. Some fancier reports might have bar graphs or flags indicating high (H) or low (L) next to abnormal values. But essentially, these are the items you’ll find in the report.
Understanding what these components mean is key to interpreting your hemogram, which we will cover next.
Understanding Your Hemogram Test Report: Interpreting Results
When you receive your hemogram test report, you’ll see a lot of numbers. It can be daunting, but understanding the gist of these results helps you have an informed discussion with your doctor. Let’s break down how to understand hemogram results parameter by parameter, and what it means if they’re high or low. Remember, normal ranges may be provided next to your results; use them as a guide and note that slight deviations might not always signify a problem – your doctor will interpret in context. Below, we outline typical interpretations:
Red Blood Cells and Hemoglobin Results
Hemoglobin (Hb) and Hematocrit (Hct): These are primary indicators of anemia or polycythemia.
- ⚫ Low Hemoglobin / Low Hematocrit (Anemia): If your hemoglobin and hematocrit are below the normal range, you have anemia. The severity can range from mild to severe depending on how low the values are. Common causes include:
- ⦿ Iron deficiency (most common, due to poor diet or chronic blood loss such as heavy menstrual periods or gastrointestinal bleeding).
- ⦿ Vitamin B12 or Folate deficiency.
- ⦿ Chronic diseases (kidney disease often causes anemia, as do some chronic inflammatory conditions).
- ⦿ Bone marrow disorders or acute blood loss (like an accident or surgery).
- ⚫ Symptoms of anemia often include fatigue, weakness, shortness of breath on exertion, dizziness, pale skin. The hemogram’s RBC indices will further hint at the type: e.g., iron deficiency anemia typically shows low MCV (microcytic, small pale cells), whereas B12 deficiency shows high MCV (macrocytic). If anemia is noted, doctors may do further tests like iron studies, B12 levels, etc., to find the cause.
- ⚫ High Hemoglobin / High Hematocrit (Polycythemia): If these are above normal, it indicates the blood has too many red cells or is too concentrated. Possible reasons:
- ⦿ Dehydration: A common benign cause – if you’re dehydrated, plasma volume drops and red cells become more concentrated, making Hct/Hb appear high. Hydration fixes this.
- ⦿ Living at High Altitudes: People in high altitude environments naturally have higher hemoglobin as an adaptation to lower oxygen.
- ⦿ Smoking or Lung Disease: Chronic smokers or people with COPD may have higher Hb (body compensates for less efficient lungs by making more RBCs to carry oxygen).
- ⦿ Polycythemia Vera: A rare bone marrow disorder that causes excessive RBC production.
- ⦿ Doping (Athletes): Use of erythropoietin (EPO) or similar to enhance performance can raise Hb.
- ⚫ High hematocrit makes blood thicker and can increase risk of clots, so if values are extremely high, doctors pay attention. They might perform a test for the JAK2 mutation (for polycythemia vera) if they suspect a bone marrow cause.
RBC Count: Usually goes hand-in-hand with Hb/Hct interpretation. Low RBC count means anemia; high means polycythemia. Sometimes, the RBC count and Hb can diverge in certain conditions (like thalassemia minor can have many RBCs but low hemoglobin per cell). But generally, you interpret RBC count similarly – low = anemia, high = polycythemia.
RBC Indices (MCV, MCH, MCHC, RDW): These help categorize the anemia:
- Low MCV (microcytosis) + low MCH often = iron deficiency or thalassemia trait.
- High MCV (macrocytosis) can mean B12/folate deficiency, alcohol liver disease, or certain medications effect.
- Normal MCV (normocytic anemia) could be anemia of chronic disease or acute blood loss.
- High RDW means variable sizes – often seen in nutritional anemias where new cells differ from old (e.g., starting iron treatment in iron deficiency can temporarily raise RDW as new cells are larger).
- Low MCHC (hypochromia) indicates pale cells, typically iron deficiency.
These details often matter more to the physician; as a patient, the main thing you note is whether you have anemia or not, and if yes, your doctor will likely explain which type based on these values. For instance, “Your hemogram shows you have anemia with small, pale red cells – likely iron deficiency, so we should check your iron levels.” That’s how a doctor uses the indices.
White Blood Cell Count and Differential Results
Total WBC Count:
- ⚫ Leukocytosis (High WBC count): If your white blood cell count is above the normal range, the cause could be:
- ⦿ Infections: Most commonly, an ongoing infection, especially bacterial, elevates WBC. WBC could be mildly elevated in a minor infection or very high in a severe infection (like appendicitis or pneumonia).
- Inflammation: Non-infectious inflammation (like autoimmune flare-ups, severe stress, even after a seizure or intense exercise) can transiently raise WBC.
- ⦿ Leukemia or Myeloproliferative disorders: Extremely high counts (e.g., >50,000) or persistent unexplained high WBC might indicate a blood cancer like leukemia. However, usually in those cases, the differential and presence of abnormal cells (blasts) in a peripheral smear give clues.
- ⦿ Medications: Drugs like corticosteroids can raise WBC count.
- ⚫ The WBC differential will usually show which type is predominantly high. For example, if neutrophils are predominantly high (neutrophilia), it aligns with bacterial infection or stress response. If lymphocytes are dominantly high, maybe a viral infection or certain chronic conditions. Eosinophilia suggests allergy or parasite, as noted.
- ⚫ Leukopenia (Low WBC count): If total WBC is below normal:
- ⦿ Viral infections: Many viral infections (like influenza, dengue, hepatitis) can transiently suppress white cell production, causing a low count during the illness.
- ⦿ Bone marrow suppression: Causes include certain medications (chemotherapy is notorious for this), radiation, or bone marrow disorders (aplastic anemia, some leukemias initially).
- ⦿ Immunodeficiency: Severe immune system problems or advanced HIV can lower WBC counts.
- ⦿ Nutritional deficiencies: Severe deficiencies (like B12 or folate) can also reduce white cell production.
- ⚫ Low WBC can increase infection risk if significantly low (especially neutrophils). Doctors might investigate persistent leukopenia to ensure there’s no serious underlying issue. Mild leukopenia might just be normal variation for some individuals or due to a recent viral infection from which you will recover.
Differential Count Interpretations: The differential gives nuanced information:
- ⚫ High Neutrophils (Neutrophilia): Suggests bacterial infection, acute inflammation, tissue damage (like heart attack or burn), or stress response. Also common if you’re on steroids. Sometimes seen in leukemia (CML or CNL).
- ⚫ Low Neutrophils (Neutropenia): Raises concern for increased risk of infections (especially bacterial). Can result from bone marrow suppression, certain drugs (some antibiotics, chemotherapy), or severe infections that overwhelm and deplete neutrophils.
- ⚫ High Lymphocytes (Lymphocytosis): Common in viral infections (e.g., mono, viral hepatitis). Also seen in certain leukemias/lymphomas (like CLL – chronic lymphocytic leukemia – where WBC count can be very high with mostly lymphocytes). Tuberculosis and some other chronic infections can cause lymphocytosis as well.
- ⚫ Low Lymphocytes (Lymphopenia): May occur in autoimmune conditions like lupus, in immunocompromised states, or due to corticosteroid use. Severe lymphopenia can be seen in advanced HIV.
- ⚫ High Monocytes (Monocytosis): Can indicate chronic infection (like TB or endocarditis), recovery phase of an acute infection, or certain blood disorders. Monocytes often increase as neutrophils recover.
- ⚫ High Eosinophils (Eosinophilia): Think allergies (asthma, eczema, hay fever) or parasites (worm infections). Also, some drug reactions and certain rare conditions (like eosinophilic syndromes, Hodgkin’s lymphoma) cause eosinophilia.
- ⚫ High Basophils (Basophilia): Rarely isolated in common conditions, but could be seen in chronic myelogenous leukemia (CML) or other myeloproliferative disorders, or hypothyroidism. Basophils are usually low in number normally, so slight increases are often not heavily emphasized unless significant.
- ⚫“Left shift”: You might hear this term – it refers to seeing more young neutrophils (bands) in blood, typically in acute bacterial infection when bone marrow is pushing out cells quickly. Automated counts sometimes flag immature granulocytes if present.
Example Interpretation: Suppose your hemogram shows WBC 15,000 with 80% neutrophils. This strongly suggests a bacterial infection or acute inflammation; your doctor might correlate with your symptoms (maybe you have a fever and cough – likely pneumonia). Conversely, WBC 3,000 with low neutrophils would alert the doctor to potential neutropenia – they may check if you’ve been ill recently or on any new medications.
If anything unusual appears in the differential (like blast cells, which are immature precursors, or atypical lymphocytes), often the lab will either automatically perform a peripheral smear review or note it. A peripheral blood smear (a slide of blood examined under microscope by a pathologist) may be recommended if the automated counts are abnormal or flags appear. This can reveal things like malaria parasites, abnormal cells, or confirm platelet counts by manual review. In a “Complete Hemogram” package, some labs include a pathologist’s review of a smear if indicated.
Platelet Count Results
Low Platelets (Thrombocytopenia): If your platelet count is below the normal range:
- ⚫ Mild thrombocytopenia (say 100k–150k) might not cause symptoms but warrants finding the cause.
- ⚫ More severe (<50k>
- ⚫ Causes include:
- ⦿ Dengue or Viral fevers: Dengue fever famously drops platelets. Other viral illnesses can too.
- ⦿ Immune thrombocytopenic purpura (ITP): an autoimmune condition where antibodies destroy platelets.
- ⦿ Aplastic anemia or bone marrow failure: where all blood cell lines (including platelets) are low.
- ⦿ Leukemia or cancers infiltrating bone marrow: they can crowd out platelet production.
- Medications: Some drugs (heparin, quinine, certain antibiotics or anti-seizure meds) can cause low platelets.
- ⦿ Liver disease: Severe liver issues can cause low platelets due to spleen enlargement or reduced thrombopoietin.
- ⚫ Your doctor will correlate a low platelet count with clinical context. If unexpectedly low, sometimes repeating the test is done, as lab error or platelet clumping can falsely lower count. If confirmed, further tests (like checking for dengue or performing bone marrow tests in severe cases) might be needed.
High Platelets (Thrombocytosis): If platelet count is above normal:
- ⚫ Reactive thrombocytosis: Most common cause, where another condition triggers it. Examples: after major surgery, trauma, or infection, platelets can rise temporarily. In inflammatory conditions (like rheumatoid arthritis or inflammatory bowel disease), platelets often go up. Iron deficiency anemia can also cause high platelets (interestingly).
- ⚫ Myeloproliferative disorder: Primary thrombocytosis, such as Essential Thrombocythemia, is a bone marrow disorder making platelets very high (often >1 million). These patients need evaluation because very high platelets can cause clotting issues and require treatment to bring counts down.
- ⚫ Post-splenectomy: People who have had their spleen removed often have elevated platelet counts since the spleen is involved in platelet storage and removal.
High platelets might not cause any symptoms, or in some cases, it could lead to headaches, dizziness, or clotting problems (clots in vessels) if extremely high. The approach depends on how high and what the suspected cause is. Slightly above normal (e.g., 500k) in the context of recent infection may just be monitored. Very high and persistent might need referral to a hematologist.
Often, platelet and WBC changes can go hand in hand or be independent. For example, an infection might raise WBC and platelets (both being acute phase reactants).
ESR (Erythrocyte Sedimentation Rate) and Its Significance
The ESR is a bit different from the above since it’s not about cell counts but rather the behavior of red blood cells in a tube. Here’s how to interpret ESR:
- ⚫ Normal ESR: Typically, an ESR of 0–20 mm/hr (some references use 0–15 for men, 0–20 for women as upper limits, as women can have slightly higher normal ESR). Children generally have very low ESR normally. If your ESR is, say, 5 mm/hr, that’s very normal – it suggests no significant inflammation at the time of testing.
- ⚫ High ESR: An elevated ESR indicates the presence of higher levels of inflammation-related proteins (like fibrinogen, immunoglobulins) that cause RBCs to clump together and fall faster in the tube. It’s a nonspecific marker, meaning it can be elevated in a wide range of conditions:
- ⦿ Infections: Especially chronic or severe infections – for instance, tuberculosis often causes a markedly high ESR. A lingering lung or bone infection could elevate ESR.
- ⦿ Inflammatory diseases: Autoimmune diseases like rheumatoid arthritis, systemic lupus erythematosus (SLE), or polymyalgia rheumatica can cause very high ESR values. In polymyalgia and temporal arteritis, ESR can be >50-100.
- ⦿ Chronic Kidney Disease: Often associated with higher baseline ESR.
- ⦿ Cancers: Certain cancers, particularly lymphomas or advanced cancers, can elevate ESR.
- ⦿ Anemia: Interestingly, having anemia can itself raise ESR (because with fewer RBCs, they sediment faster in tests).
- ⚫ The extent of ESR elevation often correlates with severity of inflammation but not always precisely. Values >100 mm/hr are considered very high and usually indicate a significant problem that needs investigation (like serious infection or autoimmune flare).
- ⚫ Mildly Elevated ESR: Sometimes ESR comes just slightly above normal (e.g., 25 or 30). This could be due to a mild inflammation (like a passing cold or slight tooth abscess), pregnancy (ESR tends to rise in pregnancy), or even age (elderly can have mildly higher ESR naturally). Doctors interpret ESR alongside CRP (C-reactive protein, another inflammation marker) if both are done, and in context of symptoms. ESR by itself doesn’t pinpoint a disease; it just signals something might be going on that merits attention.
One should note that ESR is a slower indicator – it doesn’t rise or fall quickly. CRP is more immediate. For chronic conditions, ESR is fine. For acute changes, CRP is often used nowadays. But many doctors still value ESR in assessing chronic inflammation levels.
Interpreting Combined with Hemogram: In a complete hemogram report, if you see a high ESR along with, say, high WBC and neutrophils, it strongly supports an infection/inflammatory process. If ESR is high but CBC is otherwise normal, it could be a more subtle chronic issue (or something like anemia influencing ESR). If both ESR and CRP are high (if CRP was tested), that definitely indicates active inflammation.
Example: An ESR of 50 mm/hr in a patient with known rheumatoid arthritis would suggest active disease inflammation. An ESR of 50 in someone with fever and cough might suggest pneumonia or TB and prompt further tests like a chest X-ray. Doctors also use ESR to monitor disease: e.g., if you’re on treatment for an autoimmune disease, a dropping ESR over months indicates improvement.
Putting It All Together
A hemogram test report is best interpreted by looking at patterns across these parameters:
- ⚫ If multiple related values are off (e.g., low RBC, low Hb, low Hct all consistent with anemia), the picture is clear.
- ⚫ If WBC and differential point to infection, the doctor correlates clinically (symptoms, site of infection).
- ⚫ If only one isolated value is slightly off, often it may be a quirk or lab variation; usually, significant health issues reflect in multiple parameters.
Consulting Your Doctor: It’s always recommended to discuss your hemogram results with your physician, because what’s “normal” can slightly vary based on your individual context. For instance, a hemoglobin of 12.8 g/dL might be flagged low for a male by some labs (cutoff 13), but your doctor might consider it essentially normal if everything else is fine and you feel well. Or a WBC of 11,000 (slightly above normal) might not worry them if you just recovered from a cold.
Trends: Sometimes, trends are more telling than a single result. If you have serial hemograms, doctors will compare – is your hemoglobin dropping over time? Are your platelets slowly rising over years? This can indicate a developing condition and is one reason annual check-ups help – you can catch trends.
Finally, remember that hemogram results are pieces of a puzzle. They often need to be interpreted with other tests and clinical findings. For example, if anemia is found, the next step is finding out why (which may involve checking iron levels, B12, etc.). If high WBC, finding the source of infection or performing a bone marrow test in unclear cases might be next. The hemogram gives valuable clues and sometimes outright answers, but it’s usually part of a broader diagnostic process.
If your hemogram report is completely normal, that’s great news – it means at that moment, your blood cell profile shows no signs of anemia, infection, or blood disorder. It’s a good indication of health, though of course no test covers everything.
In summary, to understand a hemogram report, check which values are out of range and in what way (high or low), then consider what conditions cause those changes. We’ve outlined the key possibilities above. Always follow up with your healthcare provider for an accurate interpretation tailored to you.
HMG Test Full Form and Terminology
You may have noticed the term HMG test appearing in conversation or on lab order forms. This is simply a shorthand for Hemogram. The full form of HMG test is “Haemogram” (with HMG representing the consonants of the word). In some lab systems or healthcare apps, they use “HMG” as an abbreviation for the complete hemogram test.
It’s important not to confuse this with other medical abbreviations. For instance, in fertility medicine, HMG can stand for human menopausal gonadotropin (a fertility drug), but in the context of blood tests, HMG clearly refers to Hemogram.
So if you want to book an HMG test, you are booking a hemogram/CBC test. Occasionally, people also use “Hgm test” or “HMG” informally when referring to the hemogram. On lab reports or results, you might not see “HMG” explicitly written; you’ll see the individual parameters as described earlier.
Another related terminology:
- ⚫ CBC stands for Complete Blood Count (the same test).
- ⚫ CBP stands for Complete Blood Picture (another synonym).
- ⚫ Complete Hemogram – as discussed – implies the CBC plus ESR.
All these names refer to overlapping concepts of a blood cell analysis. The key is knowing they are all assessing your blood cells in detail.
If you ever see “Hmg test full form?” in a question, now you know the answer: Hemogram. This clarity can help ensure you’re getting the correct test when booking online or discussing with healthcare providers.
Cost of Hemogram Test: Hemogram Test Price and Factors Affecting It
The hemogram test price can vary depending on where you get it done, your geographic location, and what exactly is included. Fortunately, the hemogram (CBC) is a relatively affordable test in most areas because it’s so commonly performed and highly automated. Here we’ll discuss typical cost ranges and factors that influence the hemogram test cost.
Compare Cost: Click Here
Factors Affecting Cost:
- ⚫ Location: Urban vs rural, region-wise differences due to cost of living and competition.
- ⚫ Lab Infrastructure: Labs with advanced equipment, accreditation (NABL/CAP accreditation in India for quality) might have slightly higher fees but ensure accuracy.
- ⚫ Home Service: Convenience sometimes adds to cost, but many labs waive it.
- ⚫ Competition and Offers: In a city with many labs, you’ll see lower prices due to competition. Online aggregators also push prices down by comparing services.
- ⚫ Volume: If a clinic or doctor’s office collects samples and sends to a lab, they might have a contract price. For individuals, you pay the list price unless you’re part of some group or scheme.
Hemogram Test Cost vs. Value: Considering the wealth of information a hemogram provides about your health, it’s generally good value for money. With one affordable test, you screen for anemia, infections, and more. This is partly why doctors order it so freely – it doesn’t usually burden the patient financially, yet it can yield critical clues.
If cost is a concern, you can shop around a bit in your locality or through health apps – but always ensure the lab is reliable. Sometimes, extremely low prices could be a red flag if the lab cuts corners. However, many certified labs manage low costs by automation and volume without compromising quality.
In summary, the haemogram test price is usually quite reasonable. In India, you’re typically looking at a few hundred rupees at most (which is roughly $4–$8 USD as of current exchange rates), and often less with discounts. In other countries:
- ⦿ In the US, a CBC might be billed higher if going through insurance (maybe $20-$50 or more list price), but insurance often covers it preventive or diagnostic. Out-of-pocket at a lab could be in a similar range of $10-$30 if directly purchased.
- ⦿ In Europe, often national health services cover it, or the cost is nominal.
- ⦿ Always check if the cost quoted to you is for the complete hemogram test (with ESR) if that’s what you need. If it just says CBC and you want ESR too, ask if there’s extra charge.
Most doctors or labs will clarify the cost upfront. Don’t hesitate to ask “How much will the hemogram test cost?” when getting it done – healthcare providers understand cost is a practical concern for patients.
Frequently Asked Questions (FAQs) about Hemogram Tests
Q1. What is the full form of the HMG test?
A1. The full form of HMG test is Hemogram (or Haemogram). HMG is simply a short abbreviation some use to refer to the hemogram test. It is the same as a complete hemogram/CBC blood test which measures all the major blood cells. So, if you see HMG on a lab requisition or search, it means a hemogram blood test.
Q2. What does a hemogram test mean, and is it different from a CBC?
A2. A hemogram test means a comprehensive analysis of your blood’s cellular components – essentially it is a complete blood count (CBC) often combined with an ESR. In most cases, hemogram and CBC are used interchangeably, with the subtle difference that “hemogram” (especially complete hemogram) usually implies CBC + ESR. Practically, if a doctor asks for a hemogram, you will get the same measurements as a CBC (RBC, WBC, differential, platelets, etc.), and often an ESR too. There’s no difference in the blood sample or procedure, just terminology and completeness of included tests.
Q3. What is included in a complete hemogram test list?
A3. A complete hemogram test typically includes:
- ⦿ Red Blood Cell (RBC) count
- ⦿ Hemoglobin (Hgb)
- ⦿ Hematocrit (Hct or PCV)
- ⦿ RBC indices (MCV, MCH, MCHC, RDW)
- ⦿ White Blood Cell (WBC) count (total leukocyte count)
- ⦿ WBC Differential (percentage/absolute count of neutrophils, lymphocytes, monocytes, eosinophils, basophils)
- ⦿ Platelet count (thrombocyte count)
- ⦿ Often ESR (erythrocyte sedimentation rate) as part of a “complete” hemogram.
Some reports may also include Mean Platelet Volume (MPV) and other platelet indices. Essentially, it’s a complete blood count with a detailed breakdown of cell types and an inflammatory marker (ESR).
Q4. Do I need to fast before a hemogram test?
A4. No, fasting is not required for a hemogram test. You can eat and drink normally beforehand. The test measures your blood cells, which are not acutely affected by eating. However, if your hemogram is part of a bigger panel of tests (like a full health check package that includes cholesterol or glucose tests), you might be asked to fast for those other tests. In such cases, it’s convenient to do all tests with one fasting sample. But for the hemogram alone, fasting is not needed.
Q5. How long does it take to get the hemogram test report?
A5. Hemogram tests are usually quick to process. In many laboratories, you can get the results the same day, often within a few hours. If you go in the morning, results are frequently ready by afternoon or evening. Some labs even provide reports within an hour or two if marked urgent. With home collection services, they often email the report by next morning at the latest. Always ask your lab – but generally, expect the report within 24 hours or sooner.
Q6. What are the normal ranges for a hemogram test?
A6. Normal ranges can vary slightly by lab and units, but approximate adult reference ranges are:
- ⦿ Hemoglobin: 13.5–17.5 g/dL (males), 12.0–15.5 g/dL (females). (Children have different ranges by age; newborns have higher, which normalize as they grow.)
- ⦿ RBC count: 4.5–5.9 million/µL (males), 4.0–5.2 million/µL (females).
- ⦿ Hematocrit: 40–50% (males), 35–45% (females).
- ⦿ WBC count: 4,000–10,000 per µL (sometimes noted as 4.0–10.0 x10^3/µL).
- ⦿ Differential: Neutrophils ~40–70%; Lymphocytes ~20–40%; Monocytes ~2–10%; Eosinophils ~1–6%; Basophils <1>
- ⦿ Platelet count: 150,000–450,000 per µL.
- ⦿ ESR: 0–15 mm/hr (males), 0–20 mm/hr (females) (and can be slightly higher with age).
Always check the reference range provided by your lab, as there are minor differences in calibration. For instance, some labs list WBC up to 11,000 as normal, or hemoglobin slightly different by population. Also, “normal” for an individual might differ (e.g., someone living at high altitude might normally have Hb ~18 which is high for sea level but normal for them).
Q7. My hemogram report showed some values slightly out of range, should I be worried?
A7. Not necessarily. Slight deviations from the reference range are common and can be due to benign factors. For example, a hemoglobin of 11.8 in a female (slightly low) could be just mild anemia due to iron deficiency – easily correctable. A WBC of 10.5 (just 0.5 over upper limit) might occur if you were fighting a mild infection or even stress during the blood draw. Labs often flag anything outside the range, but your doctor will determine significance. They may consider repeating the test after some time or doing further investigation if the result is significantly abnormal or if you have symptoms. If you feel completely well and only have a borderline result, your doctor might just advise watching it or simple measures (like iron-rich diet for a slightly low Hb). Always discuss with your physician for context – they’ll know what’s important and what isn’t.
Q8. Can a hemogram test detect cancer?
A8. A hemogram can sometimes provide clues suggestive of certain cancers, particularly blood cancers (leukemias, lymphomas, myeloma). For example, leukemia might present with extremely high WBC counts or the presence of abnormal immature cells (blasts) on the differential. Lymphomas or solid cancers can cause anemia or high platelet counts or high ESR. However, the hemogram is not a definitive test for cancer. It can raise suspicion if something is grossly abnormal, but further specialized tests (like bone marrow biopsy, imaging, biopsies of tumors, etc.) are needed to diagnose cancer. Many cancers will not show up at all on a CBC if they haven’t affected blood cell production. So while a normal hemogram is good news, it doesn’t guarantee absence of all cancer, and an abnormal hemogram doesn’t always mean cancer either – many non-cancerous conditions cause changes. It’s one piece of the diagnostic puzzle.
Q9. Is ESR always done with a hemogram?
A9. Not always – it depends on what the doctor orders or how the lab offers the test. Complete Hemogram usually includes ESR, whereas a basic CBC might not. Some doctors specifically add “ESR” to the lab form if they want it. Many modern practices rely on CRP (C-reactive protein) for an inflammation marker instead of ESR, because CRP is more responsive to changes. But ESR is still widely used. If you want a full picture including inflammation, ensure your test is “CBC with ESR” or “complete hemogram”. The cost difference is small, and it can be useful to have both.
Q10. How often should one get a hemogram test done?
A10. There’s no one-size-fits-all answer, but general recommendations:
- ⦿ For healthy individuals with no symptoms, getting a hemogram as part of an annual health check-up is common. Some do it every couple of years. It’s a quick way to screen for any changes.
- ⦿ If you have a condition like diabetes, kidney disease, or are on certain medications, your doctor might include a CBC in your routine follow-ups (perhaps 2-4 times a year) to monitor for side effects (like medication-induced low WBC, etc.).
- ⦿ For those with known anemia being treated, or a blood condition, the frequency could be more often as advised (monthly or every few months until stable).
- ⦿ If you feel unwell with unexplained symptoms (fatigue, fever, etc.), your doctor will order a hemogram at that time irrespective of when your last one was.
In short, at least once a year is a good practice for most adults to have a baseline check. Beyond that, follow your doctor’s advice or your body’s signals (symptoms).
Q11. Can I get a hemogram test at home?
A11. Yes. Many diagnostic services now offer home sample collection. You can book the test online or via phone, and a phlebotomist will come to your home or office to draw the blood at a scheduled time. The procedure for you is the same (just sit and get your blood drawn). The sample is then taken to the lab, and you receive the report via email or app. This is very convenient if you have a busy schedule or mobility issues. Ensure you choose a reputable lab that maintains proper sample handling even with home collection. The accuracy of the test is the same as if you went to the lab, provided the sample is handled properly (EDTA tube for CBC, processed in time, etc.). Many labs do not charge extra for this service nowadays, or charge a nominal fee.
Q12. What should I do if my hemogram results are abnormal?
A12. Follow up with your healthcare provider. They will likely:
- Correlate the results with your symptoms and medical history.
- Possibly repeat the test if an anomaly is unexpected (to rule out lab error or temporary fluctuation).
- Order further tests if needed. For example, if you have anemia, they might check iron levels, B12, folate, and thyroid. If WBC is high, they might look for sources of infection (urine test, chest X-ray, etc.). If platelets are low, maybe a dengue test or other specific tests depending on context.
- They will also provide treatment or advice: e.g., start iron supplements for iron-deficiency anemia, antibiotics if an infection is evident, referral to a specialist if something like leukemia is suspected.
Do not panic if you see an abnormal value; many are treatable or transient issues. Conversely, don’t ignore significantly abnormal results – always seek medical guidance to address the underlying cause.
Conclusion
In Conclusion, a hemogram (HGM blood test) is a fundamental and highly informative investigation that examines the cellular components of blood. It holds significant value in preventive health screenings, diagnosis of medical conditions, and monitoring of ongoing treatments. By understanding what a hemogram test report shows – the meaning of each parameter and what “hemogram test means” in terms of health – patients can better engage with their healthcare and comprehend why doctors place such importance on this test.
From knowing the HMG test full form to recognizing how a hemogram compares with a standard CBC, we’ve covered the full spectrum of information: the test’s purpose, procedure, interpretation, and even the practical aspect of hemogram test price. Always remember that while this test provides critical data, it is your healthcare provider who will piece together the results with clinical context for an accurate diagnosis. Use this information as a guide, and maintain regular health check-ups. The hemogram is indeed a window into your health – an accessible, affordable, and powerful tool to ensure your blood (and by extension, your body) is in good balance.
Disclaimer: This article is intended for informational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician or another qualified healthcare provider with any questions or concerns regarding a medical condition.
By following the detailed information provided in this post, you can make the most of your Hemogram Test to stay on top of your health. Regular health checkups, combined with informed lifestyle choices and a clear understanding of your blood report, will empower you to make confident decisions about your wellness.
Your health is too important to delay. Schedule your Hemogram test today at [Your Clinic Name] and take advantage of our unbeatable prices. Compare our services with leading diagnostic labs across India, and make a well-informed choice for a healthier future!
Thank you for reading our comprehensive guide on the Hemogram Test. We hope this information has been valuable and helpful. To stay updated on more health tips and insights, subscribe to our blog and join our proactive wellness community.